Amino Acid Metabolism
Protein turnover
 The recommended minimal protein intake required to achieve nitrogen balance in healthy adults is about 50g per day, although in developed countries many people may eat double this amount. This compares with an average daily protein turnover of about 250g per day. Human proteins have very different lifetimes. Total body protein is about 11kg, but about 25% of this is collagen, which is metabolically inert. A typical muscle protein might survive for three weeks, but many liver enzymes turn over in a couple of days. Some regulatory enzymes have half-lives measured in hours or minutes. The majority of the amino acids released during protein degradation are promptly re-incorporated into fresh proteins. Net protein synthesis accounts for less than one third of the dietary amino acid intake, even in rapidly growing children consuming a minimal diet. Most of the ingested protein is ultimately oxidised to provide energy, and the surplus nitrogen is excreted, a little as ammonia but mostly as urea.
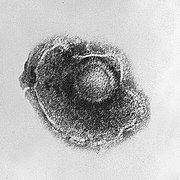
The recommended minimal protein intake required to achieve nitrogen balance in healthy adults is about 50g per day, although in developed countries many people may eat double this amount. This compares with an average daily protein turnover of about 250g per day. Human proteins have very different lifetimes. Total body protein is about 11kg, but about 25% of this is collagen, which is metabolically inert. A typical muscle protein might survive for three weeks, but many liver enzymes turn over in a couple of days. Some regulatory enzymes have half-lives measured in hours or minutes. The majority of the amino acids released during protein degradation are promptly re-incorporated into fresh proteins. Net protein synthesis accounts for less than one third of the dietary amino acid intake, even in rapidly growing children consuming a minimal diet. Most of the ingested protein is ultimately oxidised to provide energy, and the surplus nitrogen is excreted, a little as ammonia but mostly as urea.Soluble intracellular proteins are tagged for destruction by attaching ubiquitin, a low molecular weight protein marker. They are then degraded in proteasomes to short peptides. A very few of these are displayed on the cell surface by the MHC [major histocompatibility] complex as part of the immune system, but most of them are further metabolised to free amino acids. Some proteins are degraded by an alternative system within the lysosomes.
Dietary proteins are initially denatured by the stomach acid, in conjunction with limited proteolysis by pepsin. In young mammals gastric rennin [do not confuse with renin!] partially hydrolyses and precipitates milk casein and increases gastric residence time. Gastric acid also kills most ingested bacteria, rendering the upper part of the gut almost sterile.
Protein digestion is largely completed in the small intestine at a slighlty alkaline pH. The pancreatic proteases trypsin, chymotrypsin and elastase divide the proteins into short peptides. These are attacked from both ends by aminopeptidase and carboxypeptidase, and the fragments are finished off by dipeptidases secreted from the gut wall.

Glutamate and aspartate function as excitatory neurotransmitters in the central nervous system, and glutamate is partly responsible for the flavour of food. (It is the mono sodium glutamate listed on processed food labels.) However, glutamate also occupies a special position in amino acid breakdown, and most of the nitrogen from dietary protein is ultimately excreted from the body via the glutamate pool.

Transamination reactions are readily reversible, and the equilibrium constant is close to 1. One of the two pairs is almost invariably glutamate and its corresponding keto acid oxoglutarate, although there are a few exceptions to this rule. All transaminases require pyridoxal phosphate (derived from vitamin b6) as a cofactor.

Glutamate:oxaloacetate transaminase [GOT]

The metabolic importance of this enzyme is that it brings about a free exchange of amino groups between glutamate (which is the most common amino acid) and aspartate which is a second major amino acid pool. Glutamate and aspartate are each required for separate but essential steps in the urea cycle, which is responsible for ammonia detoxication and nitrogen excretion. The free movement of nitrogen between the glutamate and aspartate pools is an important balancing process that is vital for normal cellular metabolism.
Glutamate:pyruvate transaminase [GPT]

Glutamate dehydrogenase [GluDH]
This enzyme is the first committed step on the final common pathway for mammalian nitrogen excretion, leading eventually to urea. A few of the amino acids have specific deamination pathways, but about 75% of ingested protein nitrogen follows the glutamate route.

NADH / NAD and NADPH / NADP have the same standard redox potential of -420mV when the oxidised and reduced forms are present in equal concentrations. In practice these coenzymes have different effective redox potentials and perform specialised functions within cells. The NADPH / NADP pool operates almost entirely in the reduced form, but the NADH / NAD pool is rarely more than 30% reduced. In general NADPH is used to drive reductive biosynthetic reactions, whereas NAD is the coenzyme for the oxidative energy-yielding pathways.
The dual coenzyme specificity is a potential source of difficulty for the cell, since in theory this readily reversible enzyme could catalyse a futile cycle, proceeding first in the oxidative direction with NAD, followed by a reductive step using NADPH. The effect would be to "short circuit" the two coenzyme pools, which normally require considerable investment in substrates and cellular equipment to keep them separate. If this futile cycle happens to any significant extent then it must be an advantage for the cell, because it has persisted unchanged for 2,000,000,000 years of evolutionary development.
The most likely explanation at present is that this futile cycle takes place, but for various reasons it does not place an excessive burden on its owner. The Km of GluDH for ammonia is quite high, and the free ammonia concentration is kept very low by the next enzyme in the pathway, carbamyl phosphate synthetase. This will severely reduce the rate of the synthetic reaction, and allow the enzyme to catalyse a net glutamate oxidation at a slow controlled rate that provides the maximum opportunity for regulatory interference.
Regulation is plainly critical at this point, since GluDH and carbamyl phosphate synthetase jointly control the overall rate of nitrogen excretion and determine whether a particular individual will be in positive, neutral or negative nitrogen balance. Control of unwanted nitrogen losses remains an important unsolved problem after major surgery, burns or other serious traumatic injuries.
The enzyme is indeed modulated by adenine and guanine nucleotides, although it is difficult to make much sense of the observed effects. GluDH has all the hallmarks of a large multimeric allosteric enzyme, although the true nature of the regulation
The liver GluDH gene is located on chromosome 10. OMIM link Surp

It is therefore necessary to have an efficient means to remove ammonia from the body. Water-living species commonly excrete free ammonia through their gills [ammonotelism], but this easy option is not available to land dwellers which produce a variety of less toxic nitrogenous end products. Urea synthesis and excretion [ureotelism] first evolved in lungfish and primitive amphibia about 400 million years ago. The process is replicated today when ammonotelic tadpoles leave the water and metamorphose into ureotelic frogs. Urea is also used in humans, and in all placental mammals, which start to express the urea cycle genes around the time of birth. Urea is very soluble, but still requires appreciable quantities of water for its removal via the kidneys. This imposes a minimum daily water requirement and limits the range of environments that these species can exploit.
Urea is not the only possible solution to the problem: spiders excrete guanine, which packs no less than 5 surplus nitrogen atoms into a single small molecule, while reptiles and birds excrete mainly uric acid [uricotelism]. Uric acid is an extremely insoluble purine compound that readily forms supersaturated solutions. This has been turned to advantage in uricotelic species, which can survive in extremely arid environments. They regurgitate concentrated urine, supersaturated with uric acid, from the cloaca into the hindgut where the uric acid crystalises and the residual water is resorbed. The uric acid forms the fine pasty mass of white crystals that is familiar to us in bird droppings.
Uricotelism is also an advantage to animals that lay shelled eggs, which of necessity have a zero water intake. The uric acid crystalises within the allantois, part of which eventually becomes incorporated into the lower gut as the embryo develops. In humans the insolubility of uric acid is a considerable nuisance, since it gives rise to the extremely painful deposits of small crystals [called "tophi"] within the joints of patients suffering from gout.
Urea is synthesised via the urea cycle, which is confined to mammalian liver. Individual enzymes from the urea cycle are present in other tissues, and may be important for arginine biosynthesis, but the complete cycle does not occur. Extra-hepatic tissues export their surplus nitrogen to the liver by other routes, principally as the amino acids alanine and glutamine. In addition, the cleavage of arginine by nitric oxide synthetase generates citrulline, which is a urea cycle intermediate. Citrulline is recycled to arginine, and in tissues which use the nitric oxide signalling system the relevant urea cycle enzymes have sufficient activity to maintain cellular arginine supplies.
carbamyl phosphate synthetase 1 [CPS1]

CPS1 is strongly activated by N-acetyl glutamate, which controls the overall rate of urea production. This bizarre method of regulation is not fully understood: N-acetyl glutamate is an intermediate in the bacterial synthesis of ornithine, but this feature has been lost from mammals and only the regulatory system has survived. There is a futile cycle catalysed by the enzymes N-acetylglutamate synthetase and N-acetylglutamate hydrolase. This is plainly important for the control of nitrogen metabolism, but we do not yet know how it works.
ornithine transcarbamylase [OTCase]

This enzyme has no regulatory significance. However, the OTCase gene is on the X chromosome and an inherited deficiency is observed in males, with an incidence of about 1 in 80,000 people. OMIM link This is the most common of the inherited urea cycle defects. Patients show all the symptoms of hyperammonemia, and in addition may excrete abnormal amounts of orotate, since the unused carbamyl phosphate escapes into the cytosol and enters the pyrimidine biosynthetic pathway.
ornithine and citrulline porters
Glutamate and glutamate:aspartate porters


This reaction sequence is very similar to the conversion of IMP to AMP in the purine biosynthetic pathway. In each case fumarate is formed as a by-product. Fumarate is not transported by mitochondria, so this requires the presence of cytosolic fumarase to form malate.
The reaction is readily reversible, and the equilibrium slightly favours malate. The cytosolic and mitochondrial fumarase isoenzymes are extremely similar and derived from the same gene through alternative mRNA splicing reactions. OMIM link


The citrulline is reconverted to arginine using two of the urea cycle enzymes, although the full urea cycle does not take place outside the liver. See also the review by Wu & Morris mentioned above.Essential and non-essential amino acids
Humans can degrade all the amino acids that are commonly found in proteins, but we have very limited synthetic capacity. However, the initial transamination step in most of the amino acid breakdown pathways is freely reversible. If the corresponding keto acids are produced during normal metabolism, then it may be possible to use surplus nitrogen from other sources to make good a dietary deficiency in some of these "non-essential" amino acids, providing that the total nitrogen intake is sufficient.
In addition, a few amino acids are degraded to form other amino acids (for example, phenylalanine is metabolised initially to tyrosine) so that tyrosine is essential on a minimal diet, but becomes non-essential if sufficient phenylalanine is eaten. Tyrosine is therefore described as a "conditionally essential" amino acid.
Glycogenic and ketogenic amino acids
Glutamine metabolism

Glutamine supplies most of the nitrogen required for purine and pyrimidine biosynthesis, and for the manufacture of amino sugars. When necessary it can be degraded back to glutamate by the enzyme glutaminase:
Glutaminase is activated by inorganic phosphate. It is obvious that glutamine synthetase and glutaminase constitute a potential futile cycle, and the arrangment must be delicately regulated to avoid wasteful hydrolysis of ATP. The two enzymes are commonly present in different cells, and this seems to be particularly important in the liver and in the central nervous system. In liver, the urea cycle enzymes, glutamate:pyruvate transaminase and glutaminase are concentrated in the periportal cells, whereas glutamine synthetase is concentrated in the perivenous cells near the hepatic veins. See, for example, Racine et al (1995) Biochem. J. 305, 263-268; Dingemanse et al (1996) Hepatology 24, 407-411 and also Lie-Venema et al (1997) Biochem. J. 323, 611-619. Subscribers can download the last article here in Adobe pdf format.

Half of the oxygen molecule re-appears in the tyrosine -OH group and the other half is reduced to water. The "dihydrobiopterin" in the above reaction is an isomer of the folic acid compounds involved in one-carbon metabolism. It is recycled back to tetrahydrobiopterin using NADH:
Approximately one person in 45 American whites is a carrier for a defective phenylalanine hydroxylase gene, or (less frequently) the dihydrobiopterin cofactor. These mutations are particularly common in people of Celtic origin, but are less frequent in Eastern Europe. OMIM link Blood phenylalanine levels are elevated, but otherwise these heterozygotes show no symptoms and may even enjoy a heterozygote advantage. Homozygotes occur about 1 in 8,000 live births (45 * 45 * 4) and are very severely affected. Unless treated they are seriously mentally defective and excrete large quantities of phenylpyruvate in the urine. This compound gives the disease its name, and is formed by the transamination of phenylalanine, a reaction that is normally insignificant. These patients are often tyrosine deficient, and have abnormally light skin pigmentation, because they have insufficient tyrosine to synthesise melanin in normal amounts.
When this condition was first recognised in the 1930's, a significant proportion of all long term patients in mental institutions proved to be undiagnosed phenylketonuriacs. Nowadays the condition can be readily diagnosed by a heel-prick blood test performed on all new-born babies.